Comparing HSPA and CBSDP
Differences between CRCST certification and CSPDT certifications
| Healthcare Sterile Processing Association (HSPA) | CBSPD (Certification Board of Sterile Processing and Distribution) |
| CRCST CERTIFICATION: Certified Registered Central Service Technician (CRCST)
Note that both HSPA and CPSPD have a lot more certifications, but we are limiting our comparison to CRCST vs CSPDT |
CSPDT CERTIFICATION: Certified Sterile Processing and Distribution Technician (CSPDT) |
| PREREQUISTES TO TAKE CRCST EXAM
You must meet only the following conditions prior to the examination deadline: There’s no specific technical or training requirement in order to take the exam. You must submit application to HSPA to allow you to take the exam. You may apply to take the exam without enrolling in a course. Whether you self-study or enroll in a course for the exam is a decision you make.
|
PREREQUISITES TO TAKE CSPDT EXAM
You must meet only ONE of the following conditions prior to the examination deadline: · Completion of a Central Service/SPD training course with a passing grade of 70 or higher OR · Completion of 12 months of full-time employment performing SPD activities OR · Completion of 6 months (each) of fulltime employment in related clinical healthcare profession as well as performing SPD activities OR · Completion of 12 months of healthcare product sales or service related to the SPD profession |
| GETTING A CRCST CERTIFICATE
Two types of Certificates: 1. Provisional certificate is issued to those who pass the exam without hands-on experience. It is valid for 6 months 2. Full certificate is issued to those who pass the exam and obtain at least 400 hours of hands-on experience within six months of passing the exam |
GETTING A CSPDT CERTIFICATE
You become fully certified once you pass the exam. |
| Number of questions on the CRCST exam: 150 multiple choice
Time to complete CRCST exam: 3 hours Passing scaled score for the CRCST exam: 70 CRCST Exam fee: $125 exam ($150 USD outside of the US or Canada) CRCST Exam Testing center: Prometric testing |
Number of questions on the CSPDT exam: 100 multiple choice Time to complete the CSPDT exam: 2 hours Passing scaled score for the CSPDT exam: 70% grade average CSPDT Exam fee: $125 exam CSPDT Exam testing center: PSI testing |
|
CRCST RECERTIFICATION – CONTINUE EDUCATION
CRCST certificants are required to recertify annually through completion of continuing education requirements |
CSPDT RECERTIFICATION – CONTINUE EDUCATION CSPDT certificants are required to recertify every 5 years through completion of continuing education requirements |
| TO RETAKE THE CRCST EXAM
An applicant who fails any HSPA exam must wait a minimum of 6 weeks before being allowed to retest. But can submit retest application immediately upon failing the test. |
TO RETAKE THE CSPDT EXAM
An applicant who fails the CBSPD exam can retake the exam at the next test date. There are only 4 test dates available in a year |
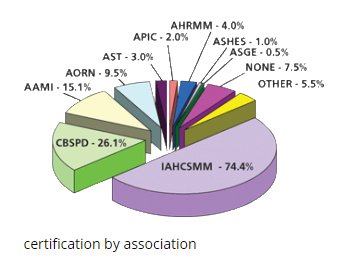
| CRCST vs CSPDT WHICH IS MORE PREFERRED BY EMPLOYERS
The answer depends on who you ask. Both certifying agencies are accredited, recognized globally and are accepted at most hospitals and surgery centers across the country. Below are answers from some Sterile processing technician job seekers: Ø Many travelers I have encountered say HSPA is more accepted across the nation Ø In my experience seeking employment, I have found that unfortunately, at least in New York, CBSPD is absolutely less well regarded than HSPA, and have been told as much in the few interviews I have had. In fact, many job postings specifically state that they require the HSPA certification My personal advice: Check career websites like indeed.com for sterile processing job postings and determine which certification has an edge as far as what certification hiring managers are requiring. |
|
| Website: www.myhspa.org | Website: www.sterileprocessing.org |
The six classes of chemical indicators are:
Class 1 process indicators
Class 2 indicators for use in specific tests
Class 3 single-variable indicators
Class 4 multi-variable indicators
Class 5 integrating indicators
Class 6 emulating indicators
Class 1: process indicators:
Class 2: indicators for use in specific tests:
The most commonly accepted type of Indicator for use in specific tests is known as a Bowie Dick indicator
Class 3: single-variable indicators: designed to react to one of the critical variables and is intended to indicate exposure to a sterilization process at a stated value of the chosen variable.
Class 4: multi-variable indicators: designed to react to two or more of the critical variables of the sterilization process. It is intended to indicate exposure to a sterilization process at specific stated values of the chosen variables.
Class 5: integrating indicators: Integrating indicators shall be designed to react to all critical variables
Class 6: emulating indicators. Emulating indicators are “cycle verification indicators” that shall be designed to react to all critical variables for specified sterilization processes
Placement of the PCD – PROCESS CHALLENGE DEVICE
Routine biological monitoring is conducted in a fully loaded chamber. The PCD should be placed on its edge if it is a small pack or flat if it is a tray or large pack. It should be positioned in the area of the sterilizer chamber and load that is least favorable to sterilization
Process challenge devices (PCDs)
A PCD is a device used to assess the effective performance of a sterilization process by providing a challenge to the process that is equal to or greater than the challenge posed by the most difficult item routinely processed.
Depending on the application in sterilization process monitoring, the PCD may contain
- a) a BI,
- b) a BI and a Class 5 integrating CI, or
- c) a Class 5 integrating CI.
- d) a Class 6 emulating indicator.
HOW TO TRANSPORT ITEMS BY HAND
Containers used to transport contaminated items by hand should be maintained in a position parallel to the floor.
The technician carrying the items should exercise good body mechanics (e.g. bend at the knees when lifting an item, hold the item close to the body).
RINSING AFTER CLEANING
Whether manual or mechanical cleaning has been performed, the device should be thoroughly rinsed to ensure
that loosened debris and detergents are adequately removed
The final rinse should be performed with treated water that is of a quality that does not contribute to staining or contamination of the instrument.
The following may be used for final rinse: Reverse Osmosis, deionized or distilled water
USE OF BRUSH FOR CLEANING
Brushes should be clean and of the appropriate size and bristle type. Worn brushes should be discarded. Reusable brushes should be disinfected or sterilized at least daily.
TEMPERATURE OF PACKAGING MATERIAL
Before use, packaging materials should be held at room temperature [68°F to 73°F] and at a relative humidity ranging from 30% to 60% for a minimum of 2 hours.
Wrappers should be kept snug to prevent low spots that could collect condensate on the exterior of the package;
however, care should be taken not to wrap too tightly, because strike-through could occur.
PACKAGING LABELS
If a marking pen is used to label paper–plastic pouches, the labeling information should be written only on the plastic side of the pouch. If a marking pen is used to label wrapped packs, basins, instruments, or other surgical supplies, the ink should be nontoxic, and the labeling information should be written on the indicator tape or affixed labels.
Paper–plastic pouches
Paper plastic pouches should stand on edge in relation to the cart or shelf, with the paper side of one pouch next
to the plastic side of the next pouch
Powders and oils
Powders such as talc and oils cannot be steam-sterilized. They should be processed by dry heat
or commercially sterilized. This is because powders and oils are impermeable to steam
COOLING AFTER STERILIZATION
All items removed from the sterilizer after sterilization processing, including items packaged in rigid sterilization container systems, should remain on the sterilizer cart until adequately cooled. They should not be touched
during the cooling process. Rigid sterilization container systems should remain on the sterilizer cart until container surfaces are cool to the touch and can be handled safely by the operator with bare hands. The cooldown
period begins within the sterilizer chamber.
. During cooling, the sterilizer cart should be placed in a low-traffic area where there are no air-conditioning or other cold-air vents in close proximity
Although a minimum cooling time of 30 minutes is recommended, adequate cooling could require 2 hours or more Packages should not be touched until they are cool because a hand can act as a point of condensation for the warm water vapor emanating from the package, thereby creating a moist area on the outside of the package. This moist area can act as a wick to draw bacteria from the hands into the package.
STORAGE FACILITIES
Sterile items should be stored in a manner that reduces the potential for contamination. In general, the temperature in storage areas should be approximately 24°C (75°F). There should be at least 4 air exchanges per
hour, and relative humidity should be controlled so that it does not exceed 70%
Heavy instrument trays should be stored on middle shelves but not stacked for ease of handling by staff.
Outside shipping containers and corrugated cartons should not be used as containers in sterile storage areas. Shipping containers have been exposed to unknown and potentially high microbial contamination, and corrugated containers serve as generators of and reservoirs for dust; hence, shipping containers should never be allowed in the sterile storage area
Tables and carts
Transport carts and tables should be large enough for all packages to be placed securely in the appropriate position (flat) without extending beyond the edge of the cart shelf or table surface. Sterile packages that contain instrumentation and that are transported by hand should be maintained in a
position parallel with the floor.
STERILIZATION RECORDS
For each sterilization cycle, the following information should be recorded and maintained:
- a) the lot number
- b) the specific contents of the lot or load, including quantity, department, and a specific description of the items (e.g., towel packs, type/name of instrument sets);
- c) the exposure time and temperature, if not provided on the sterilizer recording chart;
- d) the name or initials of the operator;
- e) the results of biological testing, if applicable;
- f) the results of Bowie-Dick testing, if applicable;
- g) the response of the CI placed in the PCD
- h) any reports of inconclusive or nonresponsive CIs found later in the load
sterilization process monitoring
Sterilization process monitoring devices include physical monitors, CIs, and BIs. Each of these devices plays a distinct and specific role in sterilization process monitoring, and each is indispensable to sterility assurance.
- Physical monitors verify that the parameters of the sterilization cycle have been met.
- Chemical indicators verify that one or more conditions necessary for sterilization have been achieved within the package and/or at a specific location within the load.
- Biological indicators verify that the conditions at a location within the load were adequate to kill a population of microorganisms resistant to the sterilization process and demonstrate the lethality of the sterilization process. Biological indicators and, in some cases, CIs are used within a PCD, to constitute a defined challenge to the sterilization process.